A cataract is a clouding of the lens in the eye that blocks light from passing through the lens to the retina, where an image is recorded. A cataract can affect your vision, giving you blurred vision. Therefore, a cataract can cause great disturbance in your daily life for work.
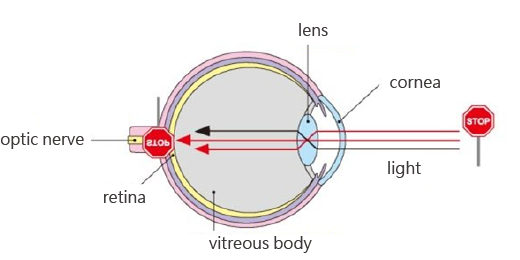
The lens is made of some chemical compositions (mostly water and protein). A cataract is when some of the protein may clump together and start to cloud a small area of the lens. Most cataracts are related to aging. Based on different causes, the types of cataracts are:
Ae-related cataract. Age-related cataract formation occurs as a result of protein clumping or lens discoloration due to exposure to ultraviolet light and tissue ageing. People can have an age-related cataract early in their 40s, which is the most common cataract type.
Congenital cataract. Some babies are born with cataracts. Congenital cataract is due to heredity, infected by rubella during pregnancy or infant metabolic disorders
Traumatic cataract. Cataracts can develop after an eye injury due to hitting, perforating, electric shock, heating, chemical burn, etc.
Secondary cataract (Complicated cataract). Cataracts can form after other eye problems or systemic disease, such as glaucoma, iritis, high myopes, diabetes, etc. Cataracts are sometimes linked to long-term corticosteroid use.
Blurred vision, double vision.
Photophobia or glares when light is shone directly
Decreased ability to differentiate colors

An old and erroneous concept goes that surgery is only necessary when the cataract becomes ‘completely ripe’, with almost complete vision loss, and even to the point of the pupil becoming white. This is completely false!
A cataract that is too mature and too hard is difficult to emulsify and remove, which will then require traditional extraction. In addition, a completely mature cataract is often with some complications such as uveitis, glaucoma, etc. In such cases, the surgery will be more complicated and will affect vision recovery.
In fact, if one encounters blurred vision and causes inconvenience in work, daily life and in leisure time, and the diagnosis, confirmed by eye doctor (ophthalmologist), is cataract. Then, the patients should consider surgery.
With the Phacoemulsification (also called "small incision cataract surgery."), a tiny probe is inserted into he lens capsule surrounding the lens. This device emits ultrasound waves that soften and break up the cloudy lens into small pieces so that it can be removed by suction via the probe. By contrast, traditional extraction surgery needs bigger incision for removing the cloudy lens.
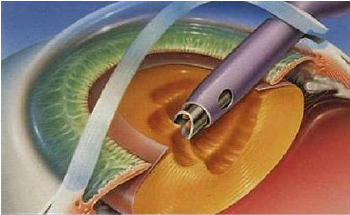
With traditional cataract surgery, a scalpel is used to make an incision on the outside of the cornea so that the turbid capsule of the lens may be opened and ultrasound is applied to crush and emulsify the lens before it is sucked out. Then, the artificial lens is placed. The so-called novel blade-free cataract femtosecond laser, on the other hand, applies the blade-less cataract femtosecond laser instead of the traditional surgical tool from the production of the corneal incision to crashing of the hardened lens.
Subsequent steps, such as the "removal of the hardened shattered lens" and "clearing of the remaining core of the lens capsule", still needs to be done through ultrasonic emulsification. Because of the reduced energy consumption and minimal harm done to the endothelial cells of the cornea, however, post-operative recovery of visual acuity appears to be even better.
Unlike the old way of making an incision manually, the blade-free cataract femtosecond laser is operated through a computer program and assisted by 3D tomography at the same time. Besides precise pre-operative positioning to show the location of the capsule, the extent of hardening of the lens, and the thickness of the cornea, and the real-time imaging also helps concurrent monitoring of the surgical status. With the traditional surgical tool replaced by the blade-free cataract femtosecond laser, the strength is that no suturing is needed after the procedure and that the patient can recover quickly!
It reduces the risk of infection and increases post-operative stability in the quality of visual acuity, realizing epoch-making surgical techniques and optimal visual quality
Novel laser technology featuring precision and exquisiteness
3D tomography real-time monitoring to prioritize safety
Exclusive tailored incision that does not need to be sutured

1. Local anesthesia
Local anesthesia is done by applying eye drops; no injection is needed and there is nearly no pain involved

2. Producing the incision
Laser is applied to produce an incision on the surface of the cornea (the primary incision, auxiliary incision, and astigmatic arc of the cornea).
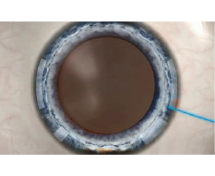
3. Circular capsule
A circular capsule is produced through femtosecond laser.

4. Crashing the core of the lens
Laser is applied to decompose the core of the lens.
5. Removing the core of the lens
Chips of the lens core are emulsified and sucked out (ultra-minimal invasive ultrasound emulsification).
6. Inserting the artificial lens
The foldout artificial lens is inserted through the incision to replace the original one.

7. Post-operative
You need to take a rest at the surgical room for 15 minutes. If no abnormalities are found, you may go home directly.

with firm fitness
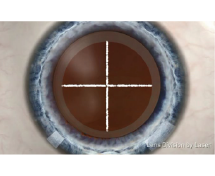
Integrating with high-resolution picture-based navigation and a complete surgical planning system, the computer is linked to a blade-free femtosecond surgical platform concurrently to keep precise control of the corneal incision, the astigmatic angle, and the center position of the artificial lens for enhanced surgical safety, precision, and quality of treatment!
The computer tailors the most suitable think center to position the astigmatic axial degree and to precisely calculate values associated with the artificial lens.
Real-time "dynamic tracking and positioning" during surgery is not affected by the shift of the eyeball.
There is precise control over the corneal incision, astigmatic angle, and the center position of the artificial lens.
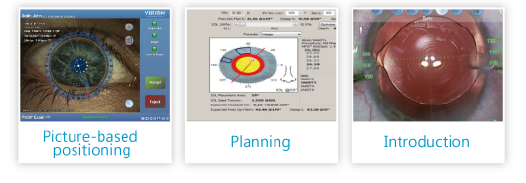
Picture-based positioning: The positioning and tracking feature during surgery
Planning: Diagnostic information is used to plan and choose the artificial lens and to stipulate a patient-exclusive surgical plan.
Introduction: Data are introduced to keep precise control over positions such as the incision and the center of the eyeball.
In a cataract procedure, the choice of artificial lens determines the post-operative visual outcome and it is therefore crucial to quality of life.
Varied artificial lenses have their distinct features and adaptability. Professional and details-oriented pre-operative exams should be done and diagnoses and assessments by the physician should be followed in order to choose a suitable artificial lens to be inserted.
Yellow VS Transparent
A yellow artificial lens is like sunglasses as it helps protect the eye by filtering out some of the harmful rays such as the blue ones and hence reduce chances of macular lesions.
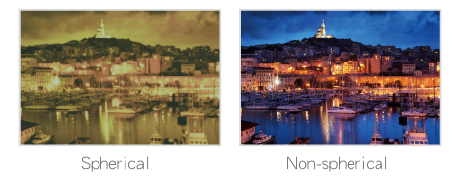
Spherical VS Non-spherical
If you need to work or drive a car or ride a bike at night, it is advised that you choose a non-spherical artificial lens as it increases your visual acuity for effectively enhanced quality of nighttime vision.
Astigmatic VS Non-astigmatic
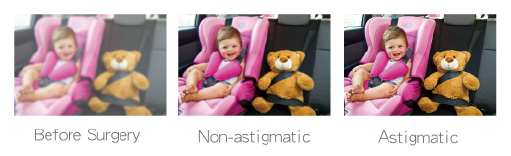
Multi-purpose Artificial Lens (Anti-presbyopia Lens Replacement)
(Adjustable for a cataract, astigmatism, presbyopia, myopia, or hyperopia!)
Polyfocal anti-astigmatism and concurrent adjustment of myopia and hyperopia nearly make your life free of dependency on glasses. It is okay for you to look at a long, medium, or short distance!
Non-spherical design, optimal nighttime vision, and anti-blue ray design reduce chances of macular lesions while at the same time precisely correcting astigmatism to ensure clear and bright vision!
After the surgery, avoid rubbing eyes with hand and holding a child in the arms in order to prevent unexpected striking and injury.
Avoid bending from the waist to tie shoelace or wash head; it is suggested to lie down when washing head, or to use a tarpaper (waterproof paper) on the forehead to prevent the water to flow into the eyes or to contaminate the upper eyelid. Avoid contacting the eyes with contaminants (e.g. face washing water, soot, etc.)
Avoid lifting heavy objects, coughing , doing strenuous exercise or looking back suddenly.
Avoid eating stimulating food to prevent coughing; drink more water and eat more vegetables and fruits to prevent constipation.
Do not worry if there is some itching and mild discomfort for a few days. Your eyes may also be a bit more sensitive to light and touch. These are normal after cataract surgery. However, if you experience a worsening of any discomfort or pain, sudden vision loss, nausea and vomiting, be sure to contact your doctor’s office immediately for examination and treatment. Be sure to follow your eye doctor's recommendation. Be sure to keep your post-operative follow-up appointment with your eye doctor.